Consumer-Directed Services
Applicable Authorities
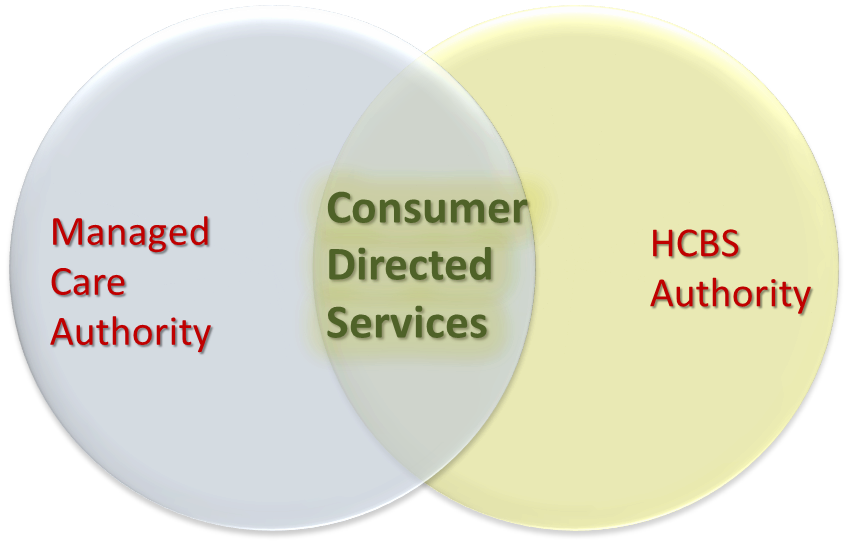
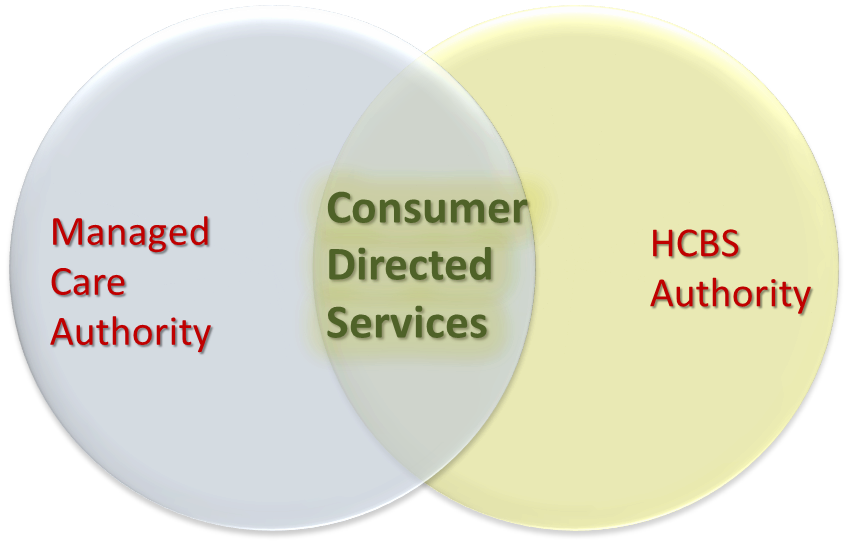
Federal Medicaid authority allows consumer-directed options through the State Plan personal care services option Section 1905(a)(24), through Section 1915(c) HCBS waivers, and through State Plan HCBS services at Section 1915(i), (j) and (k). For detailed discussion on the specific federal Medicaid requirements of offering consumer direction, see Chapter 7 of Understanding Medicaid Home and Community Services.
To incorporate consumer-directed options into your MLTSS program, you will use one or more of these HCBS authorities in combination with a managed care authority.
The managed care authority will allow you to make the option available through MLTSS contractors and to pay the contractors on a capitated basis for all MLTSS services, including those that are consumer-directed. Note that you must continue to meet the requirements of the HCBS options you are including in your program but may choose to meet some of those requirements through your MLTSS contractors. You may, for example, require your MLTSS contractor to include an existing Financial Management Services vendor in its network, and you may also require that the MLTSS contractor's network include an adequate number of agencies willing to provide the Agency with Choice model to beneficiaries.
For further discussion see the Federal Authorities section.
Below are some key issues to consider when reviewing an MCO's provider network (see 42 CFR 438.206 for a complete list of requirements):
- Adequate providers. One step in determining if a MLTSS contractor has established an adequate provider network is to review the LTSS your beneficiaries are using in the FFS environment and make sure these are well represented in the MLTSS contractor's provider network. This can ensure that the transition to managed care will yield similar access to services for consumers. Does the MLTSS contractor provider network include adequate access to skilled nursing facilities, home care providers, homemakers, etc.? Consider working with your Medicaid managed care counterparts to understand specific metrics that may be used to assess adequacy, understanding that these metrics may need to be adjusted for your target population.
- Physical accessibility. Ensure that the offices of network providers are physically accessible to beneficiaries. A few examples of physical accessibility are (1) a provider should have an elevator if their office is on the second floor, or (2) a provider should have a ramp installed if there is a step up or down into their office.
- Language access. Ensure that the provider network can accommodate your LTSS beneficiaries' language needs. This may include having providers in the network who speak languages other than English or providing access to interpreters as well as making sure providers can provide information to and communicate with beneficiaries' caregivers, beneficiaries with cognitive impairments, intellectual and/or development disabilities, and/or sensory impairments, e.g., by providing documents in braille or large print, and/or by providing access to sign language interpreters.
- Geography. In some states, beneficiary travel distance and time standards are used in Medicaid managed care programs to document reasonable access within the provider network. Consider working with your Medicaid managed care colleagues to make sure you have appropriate provisions in your LTSS solicitations/contracts, understanding that your target population may require different time and distance standards than the general Medicaid population.
- Hours of operations. The MLTSS contractor should ensure that providers have hours of operation that are appropriate for members. These hours should mirror those of commercial patients and/or of beneficiaries who have Medicaid FFS coverage.
< Back Next >